What is the primary symptom for megacolon
Hirschsprung's Disease
It is not uncommon for children with Hirschsprung's disease to continue to have problems after surgery. At Boston Children's, our gastroenterologists are dedicated to evaluating and caring for children who continue to have issues related to this disease.
These problems depend on how much unhealthy intestine needed to be removed during surgery and the current functioning of the colon, rectum, and anus.
Possible problems include:
- intractable constipation
- diarrhea
- stool accidents
- frequent episodes of infections (enterocolitis)
- recurrent hospitalizations
- severe abdominal distention (a very bloated stomach)
- pain
- inability to tolerate food
- vomiting
Children who have had a large section of intestine removed may also experience long-term digestive problems. Removing a large segment of the intestine can prevent a child from getting adequate nutrients and fluids, leading to problems with improper digestion, slow growth, and infection.
If your child still having problems following a pull-through procedure, the following tests may be done to determine what is happening:
- Anorectal manometry. This non-invasive test measures rectal nerve reflexes, which are the key indicators of Hirschsprung's disease. This is the best test to decide if your child needs to have a biopsy.
- Abdominal x-ray. This test can show signs of obstruction, as well as swollen segments of the large and small intestine.
- Barium enema. This procedure is performed to examine the large intestine for abnormalities. A fluid called barium (a chalky liquid used to coat the inside of the organs so that they will show up on an x-ray) is given via the rectum as an enema. This provides a clearer x-ray and gives your child's doctor a better picture of what is going on.
- Biopsy of the rectum or large intestine. Your child's doctor will take a sample of the cells in your child's rectum or large intestine and look at them under a microscope.
- Colonic manometry. This test involves placing a catheter (thin plastic tube) into the colon to measure contractions.
- Colonic transit studies. This procedure uses x-rays to monitor the movement of markers through the intestine and colon.
Our team will provide a thorough evaluation to locate the problem using one or more advanced diagnostic tests, such as anorectal manometry, a barium enema, or a biopsy of the rectum or colon. These tests can provide doctors with a clear picture of how the colon is working after surgery and whether the repair was successful.
Our doctors will then collaborate on a treatment plan that may include:
- medications to either slow the transit of the stool in the colon or to make it faster
- injections of Botulinum toxin (Botox) into the anal sphincter to relax this muscle
- other rectal interventions or surgical procedures that may include redoing previous operations
- further removal of abnormal intestine
- appendicostomy, a surgical procedure to flush out and empty the colon by creating an opening outside the belly
- Bowel Management Program
Complications - Ulcerative colitis
If you have ulcerative colitis, you could develop further problems.
Extra-intestinal manifestations
Around 1 in 3 people with ulcerative colitis will also develop inflammation in other parts of their body. This can lead to a range of symptoms that doctors call extra-intestinal manifestations, or extra-intestinal symptoms.
These include:
- pain, swelling and stiffness of the joints which usually happens in larger joints, such as the ankles, knees, hips and wrist
- tender bumps can appear on the skin usually on the arms and legs
- painful mouth ulcers
- eyes can become red, irritated and itchy
Osteoporosis
People with ulcerative colitis are at an increased risk of developing osteoporosis, when the bones become weak and are morelikely to fracture.
Osteoporosis can happen due to a number of factors, such as side effects of steroid medicines and the body having problems absorbing the nutrients it needs for bone growth.
It can also be caused by thedietary changes someone with the condition may take, such as avoiding dairy products, if theybelieve it could be triggering their symptoms.
If you're thought to be at risk of osteoporosis, the health of your bones will be regularly monitored.
You may also be advised to take medicine or supplements of vitamin D and calcium to strengthen your bones.
Find out more about treating osteoporosis
Poor growth and development
Ulcerative colitis, and some of the treatments for it, can affect growth and delay puberty.
Children and young people with ulcerative colitis should have their height and body weight measured regularly by healthcare professionals.
This should be checked against average measurements for their age.
If there are problems with your child's growth or development, they may be referred to a paediatrician (a specialist in treating children and young people).
Primary sclerosing cholangitis
Some people with ulcerative colitis may also develop another digestive condition called primary sclerosing cholangitis (PSC). PSC is where the bile ducts become progressively inflamed and damaged.
Bile ducts are small tubes used to transport bile (digestive juice) out of the liver and into the digestive system.
PSC does not usually cause symptoms until it's at an advanced stage.
Symptoms can include:
- fatigue(extreme tiredness)
- diarrhoea
- itchy skin
- weight loss
- chills
- a high temperature
- yellowing of the skin and the whites of the eyes(jaundice)
There's currently no specific treatment for PSC, although medicines can be used to relievesome of the symptoms, such as itchy skin.
In more severe cases, aliver transplantmay be required.
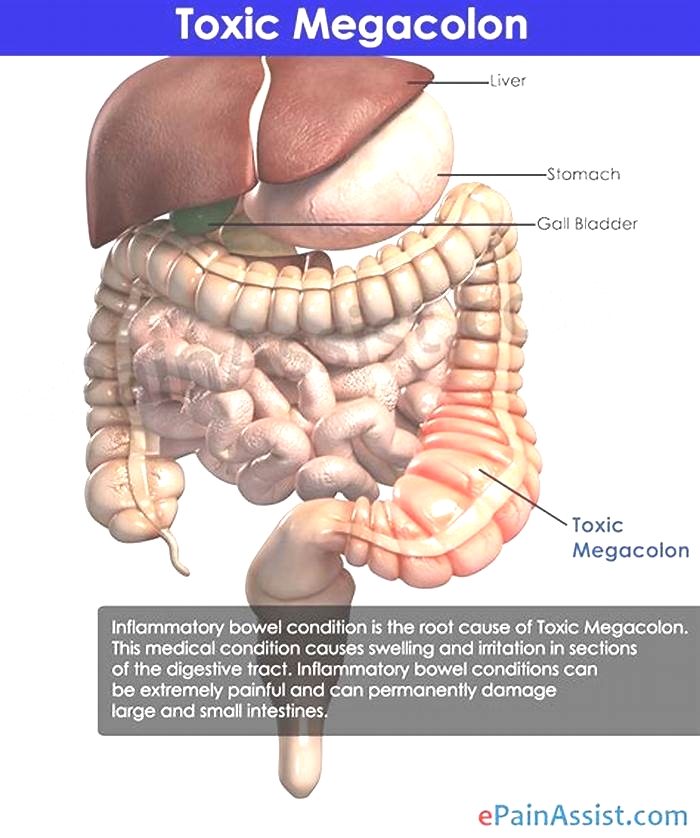
Toxic megacolon
Toxic megacolon is a rare and serious complication ofsevere ulcerative colitis where inflammation in the colon causes gas tobecome trapped, resulting in thecolon becoming enlarged andswollen.
This is potentially very dangerous as it cancause the colonto rupture (split) and cause infection in the blood (septicaemia).
The symptoms of a toxic megacolon include:
- tummy pain
- a high temperature
- a rapid heart rate
Toxic megacolon can be treated with fluids, antibiotics and steroids given directly into a vein (intravenously).
If medicines do not improve the conditions quickly, surgical removal of the colon (a colectomy) may be needed.
Treating symptoms of ulcerative colitis before they become severe can help prevent toxic megacolon.
Bowel cancer
People who have ulcerative colitis have an increased risk of developing bowel cancer (cancer of the colon, rectum or bowel), especially if the condition is severe or involves most of the colon.
The longer you have ulcerative colitis, the greater the risk.
People with ulcerative colitis are often unaware they have bowel cancer as the initial symptoms of this type of cancer are similar.
These include:
- blood in your poo
- diarrhoea
- abdominal pain
You'll usually have regular check-ups to look for signs of bowel cancer from about 10 years after your symptoms first develop.
Check-ups will involve examining your bowel with a colonoscope(a long, flexible tube containing a camera) that's inserted into your rectum this is called a colonoscopy.
The frequency of the colonoscopy examinations will increase the longer you live with the condition, and will also depend on factors such as how severe your ulcerative colitis is and if you have a family history of bowel cancer.
This can vary between every 1 to 5 years.
To reduce the risk of bowel cancer, it's important to:
- eat a balanced diet including plenty of fresh fruit and vegetables
- take regular exercise
- maintain a healthy weight
- avoid alcohol and smoking
Taking aminosalicylates as prescribedcan also help reduce your risk of bowel cancer.
Find out more about preventing bowel cancer
Page last reviewed: 01 November 2022 Next review due: 01 November 2025
Ulcerative colitis
[Music playing]
William A. Faubion, Jr., M.D., Gastroenterology, Mayo Clinic I'm Dr. Bill Faubion, a gastroenterologist at Mayo Clinic. In this video, we'll cover the basics of ulcerative colitis. What is it? Who gets it? The symptoms, diagnosis, and treatment. Whether you're looking for answers for yourself or someone you love, we're here to give you the best information available.
Ulcerative colitis is an inflammatory bowel disease that causes chronic inflammation and ulcers in the superficial lining of the large intestine, also called the colon. And that includes the rectum. It's estimated that about a million Americans are living with ulcerative colitis, making it the most common form of inflammatory bowel disease. It can be painful and debilitating, occasionally leading to severe complications. It can also be emotionally stressful. And while there is no cure, once you've been diagnosed, treatment can help you get back to a much more normal and comfortable life.
Who gets it?
The exact cause of ulcerative colitis is unknown, but there are things that appear to trigger or aggravate it. It may involve an abnormal immune response against some microorganism in which your tissues are also attacked. Genetics might also play a role. You are at higher risk if a first-degree relative has it. There's also a correlation with age. Although it can show up at any stage of life, most people are diagnosed before the age of 30. And ethnicity is a risk factor. Whites have the highest risk, especially among people of Ashkenazi Jewish descent. While diet and stress don't cause ulcerative colitis, they are known to exacerbate symptoms.
What are the symptoms?
Most people have mild to moderate cases of ulcerative colitis. Although it can be more severe, you may also experience periods of remission when you have no issues at all. A person's symptoms depend on the severity of the case in the area of the colon that's involved. They usually develop over time, and they can include diarrhea, often with blood or pus, fever, fatigue, anemia, loss of appetite and weight loss, abdominal pain and cramping, rectal pain and bleeding, the need for a bowel movement, yet the inability to do so despite the urgency. And in children, delayed growth and development. Over time, ulcerative colitis can lead to other complications, such as severe dehydration, a perforated colon, bone loss, inflammation of your skin, joints and eyes. It can also increase your risk for blood clots and colon cancer. These symptoms don't automatically mean that you have ulcerative colitis. But if you're experiencing anything that concerns you, it's a good idea to make an appointment with your doctor.
How is it diagnosed?
The only way to definitively diagnose ulcerative colitis is with a biopsy after taking a tissue sample through an endoscopic procedure. But first, less invasive things can be done to rule out other causes. First, your doctor will consider your medical history. They may want to run a variety of tests or procedures. And at some point, your general practitioner may refer you to a specialist called a gastroenterologist like myself. A blood test can check for anemia and check for signs of infection. A stool study can test for white blood cells and other specific proteins that point to ulcerative colitis, as well as rule out certain pathogens. A colonoscopy may be needed. This allows your doctor to view the entirety of the large intestine using an endoscope, a small camera mounted on a thin flexible tube. They can take tissue samples for a biopsy at the same time. Or if your colon is extremely inflamed, they may do a flexible sigmoidoscopy, which only goes as far as the rectum and lower or sigmoid colon. If your symptoms are more severe, your doctor may want some imaging done. An abdominal x-ray can rule out serious complications, like a perforated colon. An MRI or CT scan can also be performed for a more detailed view of the bowel, as well as to reveal the extent of the inflammation.
How is it treated?
Although there is no cure for ulcerative colitis there are widely effective treatments, usually involving either drug therapy or surgery. Your doctor can work with you to find things that alleviate your symptoms and in some cases, even bring about long-term remission. Treatments may include anti-inflammatory drugs like corticosteroids and immune system suppressants. Certain targeted therapies directed against the immune system called biologics can help. Antidiarrheals, pain relievers, antispasmodics and iron supplements can help counter other symptoms. And surgery may be required to remove the damaged tissue. In extreme cases, the whole colon may be removed. Which sounds drastic, but this can sometimes be the best option for eliminating the pain and struggle of ulcerative colitis once and for all. Some of these therapies may have side effects themselves. So be sure to review the risks and benefits with your doctor.
What now?
Ulcerative colitis can be physically and emotionally challenging, but there are things that can help. Although there's no firm evidence that any foods cause ulcerative colitis, certain things seem to aggravate flare-ups. So a food diary can help you identify personal triggers. Beyond that, limit dairy products, eat small meals, stay hydrated, try to avoid caffeine and alcohol and carbonation. If you're concerned about weight loss or if your diet has become too limited, talk to a registered dietitian. It's important to take care of your mental health, too. Find ways to manage stress, like exercise, breathing and relaxation techniques or biofeedback. Some symptoms like abdominal pain, gas, and diarrhea can cause anxiety and frustration. That can make it difficult to be out in public for any amount of time. It can feel limiting and isolating and lead to depression. So learn as much as you can about ulcerative colitis. Staying informed can help a lot in feeling like you're in control of your condition. Talk to a therapist, especially one familiar with inflammatory bowel disease. Your doctor should be able to give you some recommendations. And you might want to find a support group for people going through the same thing that you are. Ulcerative colitis is a complex disease, but having expert medical care and developing a treatment strategy can make it more manageable and even help patients get back to the freedom of a normal life. Meanwhile, significant advances continue to be made in understanding and treating the disease and getting us closer to curing it or preventing it entirely. If you'd like to learn even more about ulcerative colitis, watch our other related videos or visit mayoclinic.org. We wish you well.
[Music playing]